Neurospine Center of Wisconsin
__________________________________________________________________________
Definition of minimally-invasive surgery: A surgery that utilizes special tools to accomplish surgical goals through smaller incisions than conventional “open” surgery.
Benefits:



Learn more about Dr. Chabot’s background, certifications, and accomplishments:


3D-guidance to precisely place instrumentation

Spine robots utilize navigation technology to help plan surgery and place instrumentation during surgery
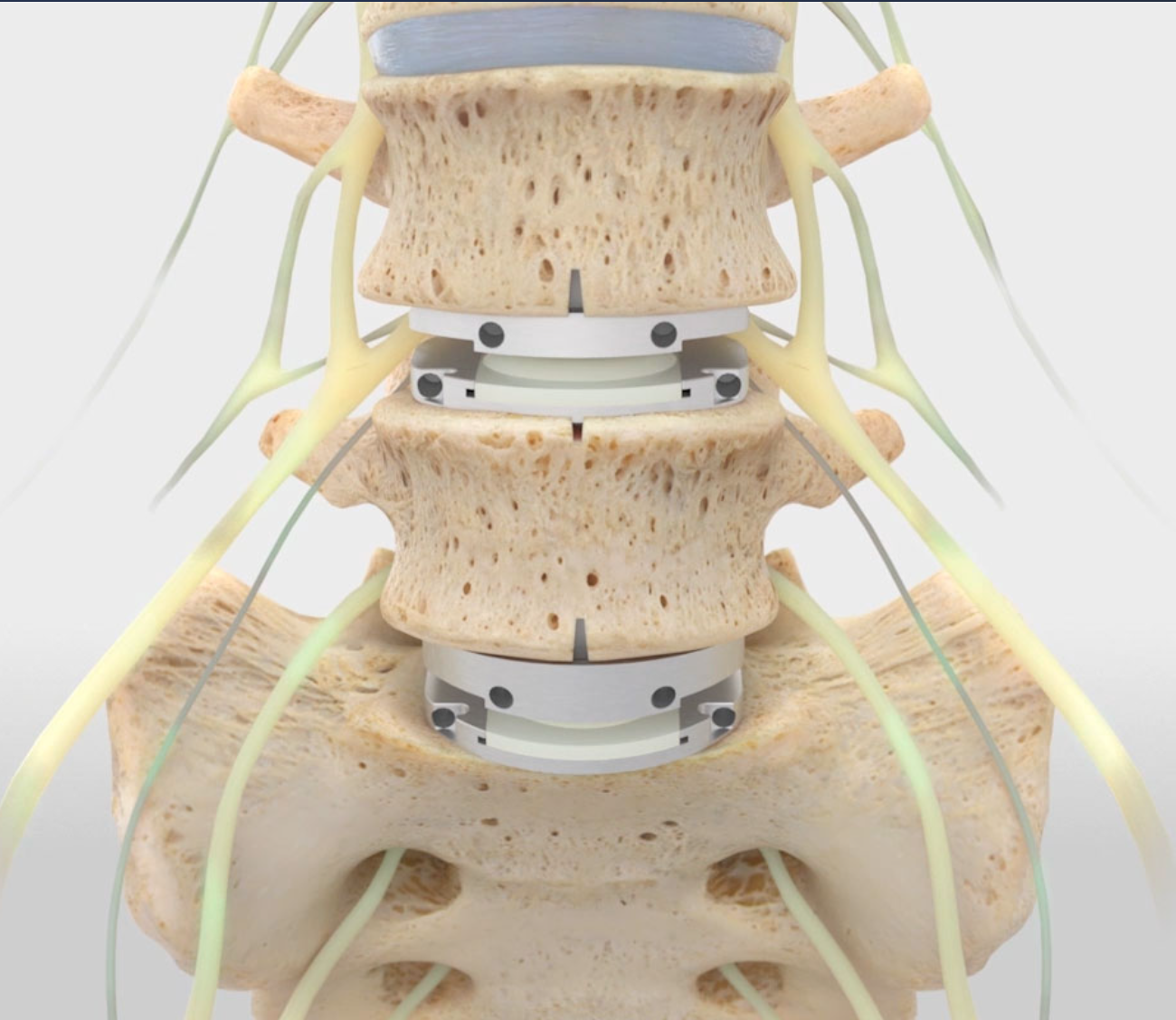
Cervical Disc Replacement-preserves the normal movement in the neck to decrease the need for future surgery

Collaboration with your team. Management of back and neck pain is a long-term relationship. Our team works with your physical therapists, chiropractor, and pain management doctor to help you avoid surgery if possible, and return you to function as soon as possible if surgery is necessary.

Identifying the correct area to treat with surgery can be challenging. By working with your existing pain management team or referring to our own team of physiatrists and anesthesiologists, we can target a precise surgical target and decrease unnecessary surgery.


There is no standard definition for “minimally-invasive spine surgery”, but more of a spectrum of invasiveness. The goal of surgery is to achieve the surgical goals with as little collateral damage as possible, but, based on comfort level, experience, or availability, newer technology designed to minimize this “surgical footprint” may not be offered by all surgeons, even those offering “minimally-invasive” options. Patients seeking a multiple opinions, should ask their surgeon what makes their surgical plan less invasive than standard open approaches.

A surgery that utilizes special tools to accomplish surgical goals through smaller incisions than conventional “open” surgery.
Most patients who are candidates for conventional “open” surgery are also candidates for minimally-invasive or motion preserving surgery. If you have been told you are not a candidate, please feel free to ask for a second opinion.
Minimally invasive surgery decreases the damage to the muscles and other soft tissues covering the spine. This can result in less blood loss, decreased post-operative pain, and faster recovery.
Anterior cervical discectomy and fusion, while a very safe and effective surgery, carries with it the 2-4% chance per year of needing surgery at other levels of the neck. Cervical disc replacements offer the same surgical results (i.e. improvement in arm and neck pain) after surgery that standard cervical fusions do, but decrease the need for future spine surgeries.
The decision to perform minimally-invasive surgeries varies from surgeon to surgeon based on their comfort level and expertise. Your surgeon should be comfortable with any surgery he or she offers, and you should be comfortable with their plan. Second opinions are always a good idea so that you can be more certain that you are making the right decision.
A surgeon’s experience and level of expertise can influence whether or not they offer you this procedure. Although there are some definite contraindications, many candidates for anterior cervical fusion are also candidates for artificial disc procedures. If you are not comfortable with your surgeon’s reasons for not offering the procedure, a second opinion may be a good idea.
Many, if not most, traditional open surgeries can also be done using minimally-invasive techniques. This includes discectomies, laminectomies, and even fusion procedures. Many surgeons offer some “minimally-invasive procedures” that are partially “minimally-invasive” and partially open. You should ask your surgeon what makes his or her procedure “minimally-invasive” as opposed to a traditional open procedure.
Many people with cervical stenosis (narrowing) involving 1 or 2 spinal levels can be treated with disc replacement (artificial disc). It is important to find a surgeon with expertise in this surgical procedure to evaluate your case and provide appropriate recommendations.
The length of recovery varies from a few days to several months based on the surgery performed. Although it may be painful to do so, walking is encouraged immediately after surgery. For larger surgeries, recovering patients may need some help around the house or may qualify for short stays in rehabilitation facilities.
Return to work usually depends on the surgery performed and the type of work. For some discectomies and cervical procedures, athletes even return to contact sports after a certain amount of time and physical therapy.
Since medications used to control pain often contribute to inattention and drowsiness, driving is often restricted while taking these drugs. Walking is encouraged, even if it is painful, since it decreases the chances of blood clots, aids in breathing and digestion, and speeds recovery.
Even the least invasive surgery requires some amount of tissue manipulation leading to inflammation and pain. In addition, the pain from compressed nerves can take time to improve even after the compression has been relieved. Pain after surgery usually decreases with time, although the amount of time varies based on the surgery performed. Additionally, back pain can be difficult to eliminate completely. Although not everyone is pain-free after surgery, the goal is to reduce the overall amount of pain so that patients can function better.
Symptoms can recur after surgery. The cause ranges from residual inflammation following surgery to re-herniation of the same disk to stenosis at other levels. Repeat surgery is not always necessary, but it is important to follow-up with your treatment team. If further surgery is not necessary, physical therapists, pain management doctors, and chiropractors can aid in your recovery.
Scarring and hardware from previous surgery can make any further surgery more difficult, but is not always a contraindication to a minimally-invasive approach. This usually depends on the comfort level and expertise of the surgeon.
The answer to this question depends entirely on the location and type of surgery performed in the cervical spine. With improved technology, there may be options available. It is best to get the opinion of a surgeon experienced in this procedure.
Yes; chiropractors often have a variety of treatment options to aid with post-operative pain or chronic pain that persists after surgery. It is important to let them know that you had surgery and where the surgery was. They will let you know if they are comfortable treating you or not, and will often seek guidance from our team regarding the appropriateness of their therapy.
A healthy, balanced diet is crucial to maintaining an appropriate weight before and after spine surgery. Since excess weight often contributes to spine degeneration, this lifestyle changes such as diet and activity can help prevent the need for future surgery. Before and after surgery, a diet high in lean proteins and calcium (some dairy, dark leafy greens) can aid in muscle and bone recovery. It may be a good idea to talk to a dietitian for specific recommendations.
Back pain is notoriously difficult to treat, and takes a long time to get better after surgery. Also, surgery to treat back pain is not always successful. If you still have pain after surgery, please followup with your surgical team to make sure everything is healing properly. Afterwards, physical therapy, chiropractors, and pain management may be able to aid with your symptoms. Some people with persistent pain after spine surgery may be a candidate for a variety of “functional” procedures, such as a “spinal cord stimulator” to help manage their pain.
The risks of minimally-invasive spine surgery are similar to open spine surgery. These include minor risks, such as post-operative pain and superficial wound issues, to more serious complications, such as weakness or nerve damage. Your surgeon should discuss these risks with you in detail prior to proceeding with any surgical procedure.
In many cases, the same degree of nerve decompression and placement of hardware can be achieved through a smaller incision than open surgery. However, there are limitations to minimally-invasive approaches that may make open surgery a better option. To get a balanced opinion, it is important to find a surgeon that is familiar with both minimally-invasive and open procedures.
Physical therapy is more than “just exercises and stretching”. Many painful spinal conditions will improve without surgery if a patient works hard at physical therapy. If surgery is still necessary, physical therapy beforehand can aid in recovery afterwards. Finally, if you have weakness before or after surgery, physical therapy is necessary to help improve this weakness and improve your overall function.
Still have questions? Contact me.