Indication: pinched nerves or compressed spinal cord in neck causing neck or arm pain and/or weakness
Description: Approaching through the front of the neck, the surgeon will remove the portions of the disc or bone spurs that are pushing on the spinal cord or nerves. A “cage” filled with graft material is placed in between the cervical vertebrae (neck bones). With time, the bones will fuse together to form a single, solid bone. Patients usually walk within a few hours after surgery, and, depending on the number of levels treated, go home the same day or the next without a neck brace.

Indication: pinched nerves or compressed spinal cord in neck causing neck or arm pain and/or weakness
Description: Approaching through the front of the neck, the surgeon will remove the portions of the disc or bone spurs that are pushing on the spinal cord or nerves. A device that mimics the natural movement of the removed disc is placed between the cervical vertebrae (neck bones). By maintaining the normal movement of the neck, the risk of needing future surgery at nearby levels may be reduced. Patients usually walk within a few hours after surgery, and go home the same day without a neck brace.

Indication: nerves in the neck pinched by protruding (herniated) cervical disks or bone spurs causing neck or arm pain
Description: The surgery is performed from the back of the neck. The muscles on the side of the spine are retracted to allow access to the cervical lamina (neck bones). A small amount of bone is removed to expose the pinched nerve. Using a microscope for magnification, any tissue pushing on the nerve is carefully detached and removed. Patients walk within a few hours after surgery, and go home the same day.

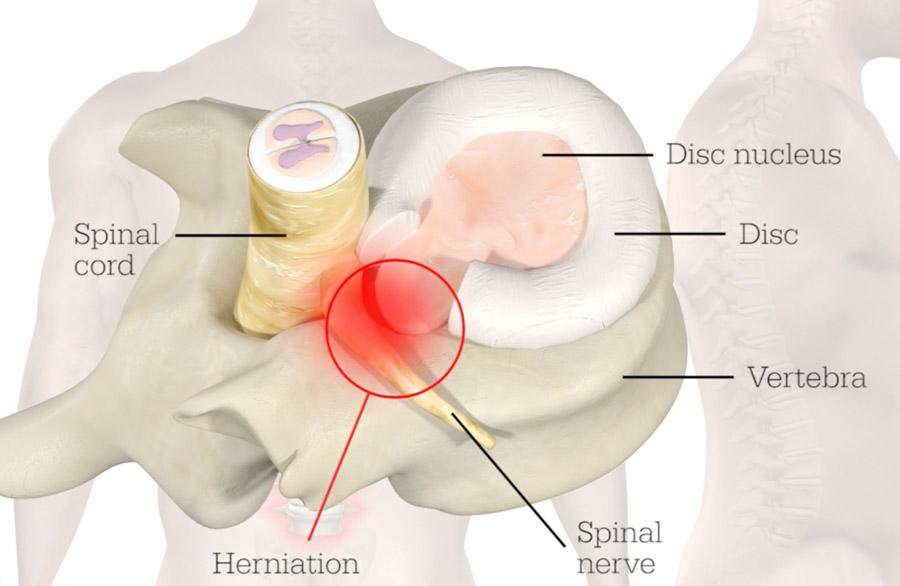
Indication: nerves in the lumbar spine (low back) pinched by a protruding disk causing back and leg pain, or “sciatica”
Description: The surgery is performed through the low back. A small tube, about the width of a coin, is inserted on top of the bones of the spine. Using a microscope focused through the tube, small pieces of bone and ligament are moved to expose the nerve underneath. The protruding disk is then cut out to free up the pinched nerve. Patients usually walk within a few hours after surgery and go home the same day.

Indication: nerves in the lumbar spine (low back) pinched by arthritis and bulging ligaments causing “sciatica” (back and leg pain) or “claudication” (leg heaviness improved by bending forward)
Description: The surgery is performed through the low back. A small tube, about the width of a coin, is inserted on top of the bones of the spine. Using a microscope focused through the tube, small pieces of bone and ligament are removed to expose the sack of nerves underneath. The tube is aimed in different directions to ensure that the entire space is well decompressed. Patients usually walk within a few hours after surgery, and go home either the same day or the next.

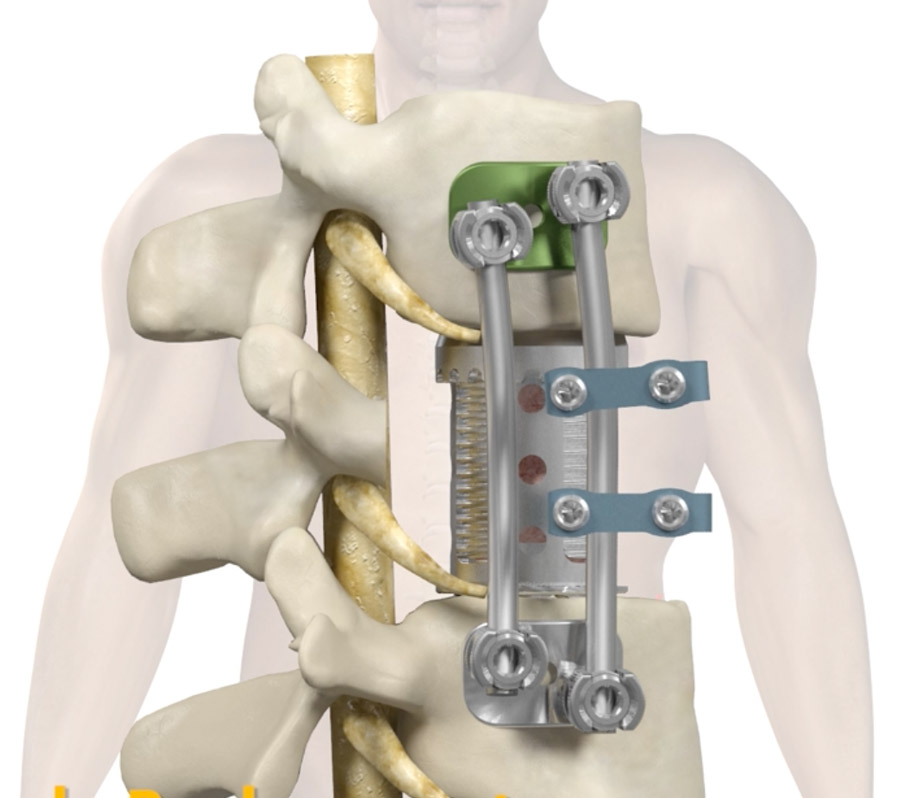
Indication: back pain caused by excessive movement between two vertebrae (spondylolisthesis) or back/leg pain in which fixating (fusing) the vertebrae is recommended
Description: The surgery is usually performed as an adjunct to a decompressive surgery (cf. minimally-invasive laminectomy, minimally-invasive discectomy, lateral lumbar fusion, anterior lumbar fusion) in which screw placement is necessary. In standard open surgery, the muscles lining the back are scraped from their bony attachments in order to expose landmarks necessary for screw placement. Robotic surgery is a form of image guidance, which allows the surgical team to see the tips of their instruments on a computer screen while utilizing a small incision. GPS for the spine is another way of describing it.
Using a CT scan obtained during surgery, the surgical team plans the ideal position for the screws or other instrumentation. A robotic arm the guides the screw and instruments safely to the planned target.
This technique allows for highly accurate screw placement while minimizing muscle disruption and blood loss. Patients usually walk within a few hours after surgery, and go home the next day.

Indication: Back pain caused by excessive movement between two vertebrae (spondylolisthesis) or back/leg pain in which fixating (fusing) the vertebrae is recommended. It may also be used as a spacer to open up a narrowed foramen (opening between two bones through which the nerve exits) to relieve a pinched nerve
Description: working in conjunction with an access surgeon, usually a general or vascular surgeon, an incision is made in the area of the belt line on the patients abdomen. A surgical corridor is developed allowing the abdominal contents to be gently retracted to expose the front of the lumbar spine. The blood vessels in front of the spine are carefully mobilized and protected. The disc is removed from in between the vertebrae and a spacer inserted with graft material that encourages bone growth. If necessary, the patient is then repositioned and screws placed using robotic assistance and a minimally-invasive laminectomy performed.
This surgery allows for placement of a much larger spacer than surgery from behind and minimizes damage to the back muscles by approaching from the front. Patients usually walk around a few hours after surgery, and go home the next day.

Indication: Back pain caused by excessive movement between two vertebrae (spondylolisthesis) or back/leg pain in which fixating (fusing) the vertebrae is recommended. It may also be used as a spacer to open up a narrowed foramen (opening between two bones through which the nerve exits) to relieve a pinched nerve.
Description: The patient is positioned on their side, usually with the left side up. A small incision is made just above the top of the hipbone. A retractor is placed through a muscle running over the side of the spine to expose the disc underneath. Specialized electric stimulation and recording devices are used to ensure that the nerves in this region are not damaged. The disc is removed from in between the vertebrae and a spacer placer inserted with graft material that encourages bone growth. If necessary, the patient is then repositioned and screws placed using robotic assistance and a minimally-invasive laminectomy performed.
Patient usually walk around a few hours after surgery, and go home the next day.This option allows for placement of a much larger spacer than surgery from behind and minimizes damage to the back muscles by approaching from the side.

Indication: Intractable back and leg pain without a clear surgical target, or persistent back and leg pain following surgery (post-laminectomy syndrome or failed back syndrome).
Description: a trial is performed working in conjunction with pain management colleagues. A temporary wire is inserted on top of the spinal cord, and tunneled though a small opening in the patient’s skin. Over a course of several days at home, the patient works with a representative from the stimulator company to use different settings to alleviate their symptoms.
The leads are then removed in the office. If the trial is successful, a permanent stimulator is placed.
This involves s small incision in the middle of the back and second incision on the right or left side of the low back. Through the first incision, a small window in the bones of the thoracic spine is made. A lead, or electrode, is placed underneath the bones to lay on top of the lining of the spinal cord.
The second incision, in the low back, is used to create a pocket underneath the skin. The electrode is tunneled from the first incision to the second incision underneath the skin, and the electrode connected to the generator.
Patients walk around a few hours after surgery and go home the same day. The generator can be recharged and programmed while remaining underneath the skin.

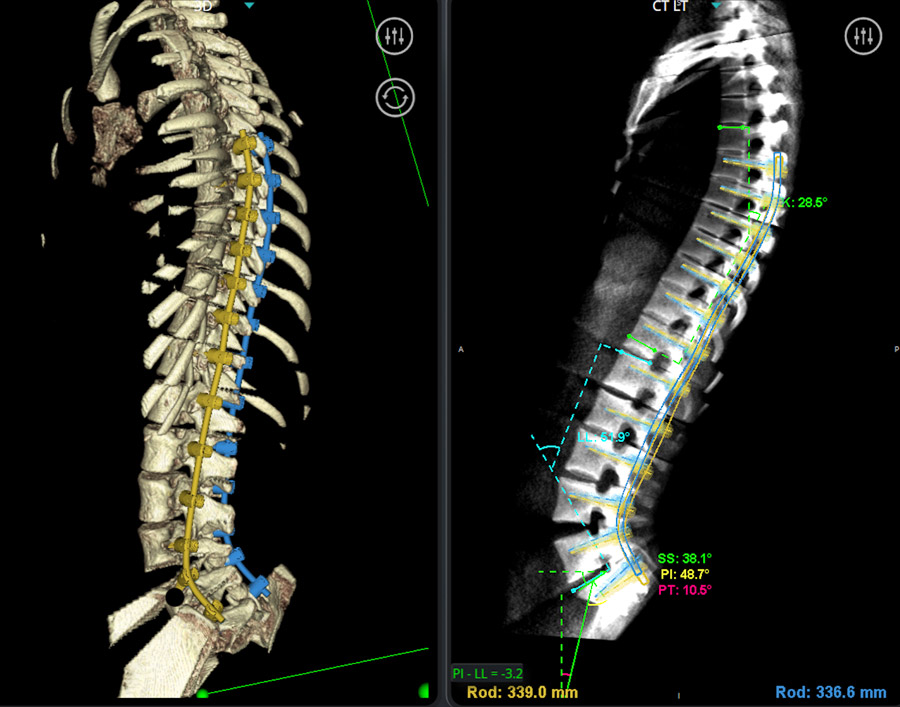
Indication: Including, but not limited, to scoliosis, spinal fractures, spinal tumors, pseudoarthrosis, revision surgery, and severe narrowing (stenosis) at multiple levels of the spine. Minimally invasive procedures may be utilized to avoid large open surgeries in select cases.
Description: the surgical approach varies based on the surgical goals and the comfort level of the surgeon with the minimally invasive options. Sometimes, minimally-invasive principles approaches may be utilized in conjunction with standard open approaches (hybrid surgery). Generally speaking, surgery requires removal of portions of bones in the spine to decompress nerve roots and placement of spacers and screws to restore alignment. Certain tools, such as computer navigation, used extensively in minimally-invasive surgery, can be used to improve the accuracy and efficiency of more complex surgeries.

Indication: Including, but not limited, to scoliosis, spinal fractures, spinal tumors, pseudoarthrosis, revision surgery, and narrowing at multiple levels of the spine.
Description: the surgical approach varies based on the surgical goals and the comfort level of the surgeon with the minimally invasive options. Generally speaking, surgery requires removal of portions of bones in the spine to decompress nerve roots and placement of spacers and screws to restore alignment. Since minimally-invasive surgery is not always appropriate for complex spine surgery, it is important for spine surgeons to be familiar with both approaches. Recovery varies based on the presenting condition of the patient and the extensiveness of the surgery.

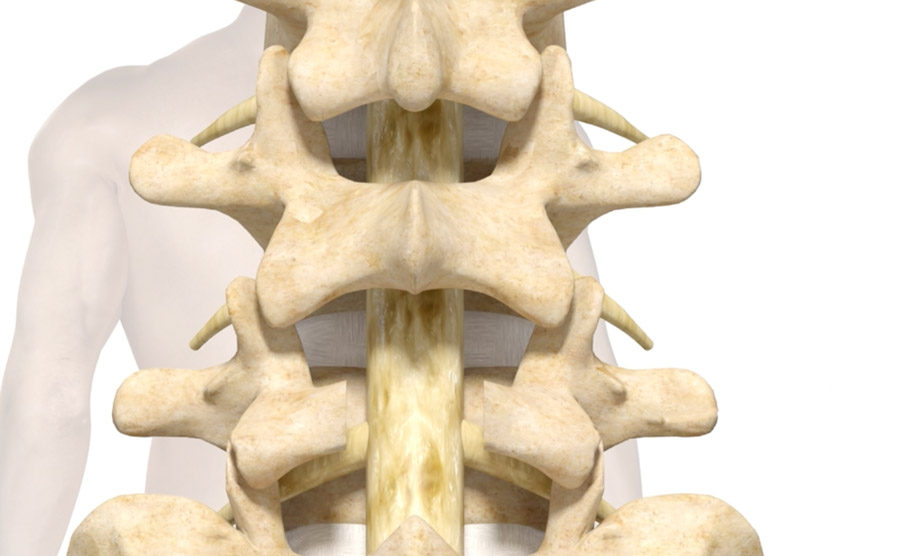
Indication: nerves in the lumbar spine (low back) pinched by arthritis and bulging ligaments, causing back and leg pain, or “sciatica” or heaviness in the leg improved with bending forward, or “claudication”. Pinched nerves or spinal cord in the neck causing neck and arm pain or weakness. Open approaches may be chosen in cases where a minimally-invasive surgery is not feasible.
Description: The surgery is performed through the low back. The bone and ligaments pinching the nerves are then removed using a drill and other instruments. A microscope may be used to aid in visualization. Patients usually walk a few hours after surgery and go home the same day as surgery or the next day.

Indication: nerves in the lumbar spine (low back) pinched by a protruding disk causing back and leg pain, or “sciatica”. Open approaches maybe utilized in cases where minimally-invasive surgery is not feasible.
Description: An incision is made in the low back. The bones overlying the nerve roots are carefully removed using drills and other instruments. Using a microscope for magnification, the compressed nerve root is exposed and mobilized to show the protruding disc underneath. The disc is then removed to decompress the nerve. Patients usually walk within a few hours after the surgery and go home the same day.

Indication: re-operation in the lumbar spine for a variety of reasons including new narrowing (stenosis) and nerve compression at levels adjacent to prior surgery, or failure of previous fusion surgery or hardware
Description: Revision surgery can be challenging due to the presence of scar tissue and the absence of anatomic landmarks. The specific surgery may vary based on the surgical goals. Computer navigation can help guide the surgeon to surgical targets obscured by scarring. Lateral and anterior approaches may be used to avoid the distortion caused by previous surgery from the back. Minimally-invasive, combined minimally-invasive and open, and standard open surgeries may be necessary. Recovery varies based on the presenting condition of the patient and the extensiveness of the surgery.

Indication: re-operation in the cervical spine for a variety of reasons including new narrowing (stenosis) and nerve compression at levels adjacent to prior surgery, or failure of previous fusion surgery or hardware
Description: Revision surgery can be challenging due to the presence of scar tissue and the absence of anatomic landmarks. The specific surgery may vary based on the surgical goals. Computer navigation can help guide the surgeon to surgical targets obscured by scarring. Recovery varies based on the presenting condition of the patient and the extensiveness of the surgery.


NueroSpine Center Of Wisconsin • Society for Minimally Invasive Spine Surgery • Cervicaldisc.com • Spine-health.com • Rediscover Spine Community